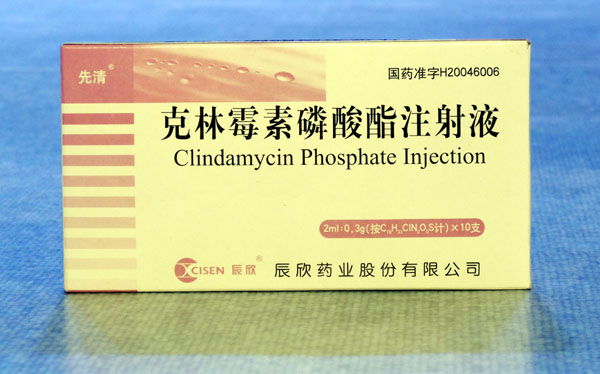
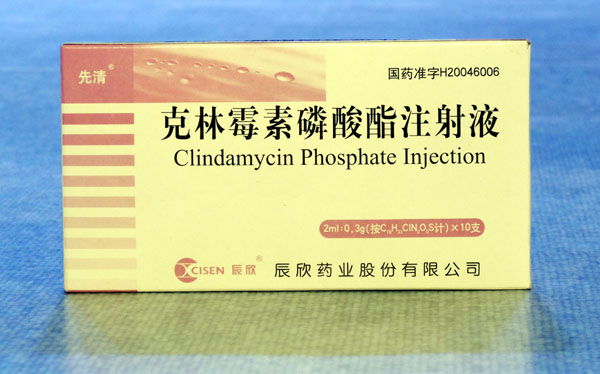
Description: Clindamycin Phosphate Sterile Solution in vials contains clindamycin phosphate, a water soluble ester of clindamycin and phosphoric acid. Each mL contains the equivalent of 150 mg clindamycin, 0.5 mg disodium edetate and 9.45 mg benzyl alcohol added as preservative in each mL. Clindamycin is a semisynthetic antibiotic produced by a 7(S)-chloro-substitution of the 7(R)-hydroxyl group of the parent compound lincomycin. The molecular formula is C18H34CIN208PS and the molecular weight is 504.96. Clindamycin phosphate in the ADD-Vantage Vial is intended for intravenous use only after further dilution with appropriate volume of ADD-Vantage diluent base solution.
Pharmacological effects: Serum level studies with a 150 mg oral dose of clindamycin hydrochloride in 24 normal adult volunteers showed that clindamycin was rapidly absorbed after oral administration. An average peak serum level of 2.50 mcg/mL was reached in 45 minutes; serum levels averaged 1.51 mcg/mL at 3 hours and 0.70 mcg/mL at 6 hours. Absorption of an oral dose is virtually complete (90%), and the concomitant administration of food does not appreciably modify the serum concentrations; serum levels have been uniform and predictable from person to person and dose to dose. Serum level studies following multiple doses of Clindamycin HCl for up to 14 days show no evidence of accumulation or altered metabolism of drug. Serum half-life of clindamycin is increased slightly in patients with markedly reduced renal function. Hemodialysis and peritoneal dialysis are not effective in removing clindamycin from the serum. Concentrations of clindamycin in the serum increased linearly with increased dose. Serum levels exceed the MIC (minimum inhibitory concentration) for most indicated organisms for at least six hours following administration of the usually recommended doses. Clindamycin is widely distributed in body fluids and tissues (including bones). The average biological half-life is 2.4 hours. Approximately 10% of the bioactivity is excreted in the urine and 3.6% in the feces; the remainder is excreted as bioinactive metabolites. Doses of up to 2 grams of clindamycin per day for 14 days have been well tolerated by healthy volunteers, except that the incidence of gastrointestinal side effects is greater with the higher doses. No significant levels of clindamycin are attained in the cerebrospinal fluid, even in the presence of inflamed meninges. Pharmacokinetic studies in elderly volunteers (61–79 years) and younger adults (18–39 years) indicate that age alone does not alter clindamycin pharmacokinetics (clearance, elimination half-life, volume of distribution, and area under the serum concentration-time curve) after IV administration of clindamycin phosphate. After oral administration of clindamycin hydrochloride, elimination half-life is increased to approximately 4.0 hours (range 3.4–5.1 h) in the elderly compared to 3.2 hours (range 2.1 – 4.2 h) in younger adults. The extent of absorption, however, is not different between age groups and no dosage alteration is necessary for the elderly with normal hepatic function and normal (age-adjusted) renal function.
Pharmacokinetics: Biologically inactive clindamycin phosphate is rapidly converted to active clindamycin.By the end of short-term intravenous infusion, peak serum levels of active clindamycin are reached. Biologically inactive clindamycin phosphate disappears rapidly from the serum; the average elimination half-life is 6 minutes; however, the serum elimination half-life of active clindamycin is about 3 hours in adults and 2.5hours in pediatric patients. After intramuscular injection of clindamycin phosphate, peak levels of active clindamycin are reached within 3 hours in adults and 1 hour in pediatric patients. Serum levels of clindamycin can be maintained with minimum inhibitory concentrations for most indicated organisms by administration of clindamycin phosphate every 8 to 12 hours in adults and every 6 to 8 hours in pediatric patients, or by continuous intravenous infusion. An equilibrium state is reached by the third dose. The elimination half-life of clindamycin is increased slightly in patients with markedly reduced renal or hepatic function. Hemodialysis and peritoneal dialysis are not effective in removing clindamycin from the serum. Dosage schedules need not be modified in the presence of mild or moderate renal or hepatic disease. No significant levels of clindamycin are attained in the cerebrospinal fluid even in the presence of inflamed meninges.
Indications: Clindamycin phosphate products are indicated in the treatment of serious infections caused by susceptible anaerobic bacteria. Clindamycin phosphate products are also indicated in the treatment of serious infections due to susceptible strains of streptococci, pneumococci, and staphylococci. Its use should be reserved for penicillin-allergic patients or other patients for whom, in the judgment of the physician, a penicillin is inappropriate. Because of the risk of antibiotic-associated pseudomembranous colitis, as described in the WARNING box, before selecting clindamycin the physician should consider the nature of the infection and the suitability of less toxic alternatives (e.g., erythromycin). Clindamycin phosphate is indicated in the treatment of serious infections caused by susceptible strains of the designated organisms in the conditions listed below: Lower respiratory tract infections including pneumonia, empyema, and lung abscess caused by anaerobes,Streptococcus pneumoniae, other streptococci (except E. faecalis), and Staphylococcus aureus. Skin and skin structure infections caused by Streptococcus pyogenes, Staphylococcus aureus, and anaerobes. Gynecological infections including endometritis, nongonococcal tubo-ovarian abscess, pelvic cellulitis, and postsurgical vaginal cuff infection caused by susceptible anaerobes. Intra-abdominal infections including peritonitis and intra-abdominal abscess caused by susceptible anaerobic organisms. Septicemia caused by Staphylococcus aureus, streptococci (except Enterococcus faecalis), and susceptible anaerobes. Bone and joint infections including acute hematogenous osteomyelitis caused by Staphylococcus aureus and as adjunctive therapy in the surgical treatment of chronic bone and joint infections due to susceptible organisms. To reduce the development of drug-resistant bacteria and maintain the effectiveness of clindamycin phosphate and other antibacterial drugs, clindamycin phosphate should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
Precautions: Review of experience to date suggests that a subgroup of older patients with associated severe illness may tolerate diarrhea less well. When clindamycin is indicated in these patients, they should be carefully monitored for change in bowel frequency. Clindamycin phosphate products should be prescribed with caution in individuals with a history of gastrointestinal disease, particularly colitis. Clindamycin phosphate should be prescribed with caution in atopic individuals. Certain infections may require incision and drainage or other indicated surgical procedures in addition to antibiotic therapy. The use of clindamycin phosphate may result in overgrowth of nonsusceptible organisms—particularly yeasts. Should superinfections occur, appropriate measures should be taken as indicated by the clinical situation. Clindamycin phosphate should not be injected intravenously undiluted as a bolus, but should be infused over at least 10–60 minutes as directed in the DOSAGE AND ADMINISTRATION section. Clindamycin dosage modification may not be necessary in patients with renal disease. In patients with moderate to severe liver disease, prolongation of clindamycin half-life has been found. However, it was postulated from studies that when given every eight hours, accumulation should rarely occur. Therefore, dosage modification in patients with liver disease may not be necessary. However, periodic liver enzyme determinations should be made when treating patients with severe liver disease. Prescribing clindamycin phosphate in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Adverse reaction: The following reactions have been reported with the use of clindamycin. Gastrointestinal: Abdominal pain, pseudomembranous colitis, esophagitis, nausea, vomiting and diarrhea (see WARNING box). The onset of pseudomembranous colitis symptoms may occur during or after antibacterial treatment. Hypersensitivity Reactions: Generalized mild to moderate morbilliform-like (maculopapular) skin rashes are the most frequently reported adverse reactions. Vesiculobullous rashes, as well as urticaria, have been observed during drug therapy. Rare instances of erythema multiforme, some resembling Stevens-Johnson syndrome, and a few cases of anaphylactoid reactions have also been reported. Skin and Mucous Membranes: Pruritus, vaginitis, and rare instances of exfoliative dermatitis have been reported. Liver: Jaundice and abnormalities in liver function tests have been observed during clindamycin therapy. Renal: Although no direct relationship of clindamycin to renal damage has been established, renal dysfunction as evidenced by azotemia, oliguria, and/or proteinuria has been observed in rare instances. Hematopoietic: Transient neutropenia (leukopenia) and eosinophilia have been reported. Reports of agranulocytosis and thrombocytopenia have been made. No direct etiologic relationship to concurrent clindamycin therapy could be made in any of the foregoing. Musculoskeletal: Rare instances of polyarthritis have been reported.